The Doctor’s Office of 2030—4 Predictions for the Future
In the past decade, significant advancements have been made in medical research and technology that have improved the overall healthcare experience for patients and made it easier for doctors to provide better, more efficient care. For example, electronic medical records (EMRs) have replaced paper files in medical practices and hospitals, and artificial intelligence (AI) is currently being used in medical chatbots to field patient questions, connect patients to clinicians, and improve patient engagement.
The question now is: What’s next on the horizon for doctors and patients? And it’s a crucial question to ask considering the potential impact these technologies could have, from improved diagnosis and treatment plans to faster, more efficient administrative processes. In order to be prepared for them in ten years, doctors must start considering them today.
Four tech predictions to prepare for today
To answer that question, we scoured Gartner research papers, talked to healthcare professionals, and used our own market knowledge to compile this list of our four noteworthy predictions for medical technology of the future.
Here are our four predictions for how healthcare technology will shape the doctor’s office of 2030:
Doctors will rely on wearable tech for real-time insights
Waiting rooms will be phased out
Up to a quarter of visits will happen virtually—or not at all
Patients will take more ownership of their personal health data
1. Doctors will rely on wearable tech for real-time insights
Wearable technology is already popular among some consumer groups, particularly fitness enthusiasts. These high-tech fitness trackers measure everything from a person’s heart rate to activity level and even sleep patterns. As this technology becomes more efficient and less obtrusive to everyday activity, experts say it will likely become a big part of the medical community, providing doctors with patients’ real-time health information.
“Current wearables such as the Cuff and the Athos fitness tracker, among many others in this space, already allow patients to monitor their own health by measuring heart rate, respiratory rate, and calories,” says Dr. Sandeep Rao, MBA.
“The next step is for the patient to be able to plug this data into their medical records, which would allow us to mine data for both individual patients and groups of patients.”
One example Dr. Rao gives is treating a large group of high blood pressure patients with a certain anti-hypertensive drug. Wearable technology would allow the doctor to track the effect of the medication on each patient’s heart rate and blood pressure.
“The physician[s] could then aggregate this data centrally, analyze it, and determine the efficacy of the medication on different demographics [women, young patients, Asians, etc.], and finally target each population with the best medication,” says Dr. Rao.
Our own research corroborates Dr. Rao’s prediction: In a survey we conducted with over 300 patients, 97% said they are interested in sharing personal data collected by wearable fitness trackers with their healthcare providers.
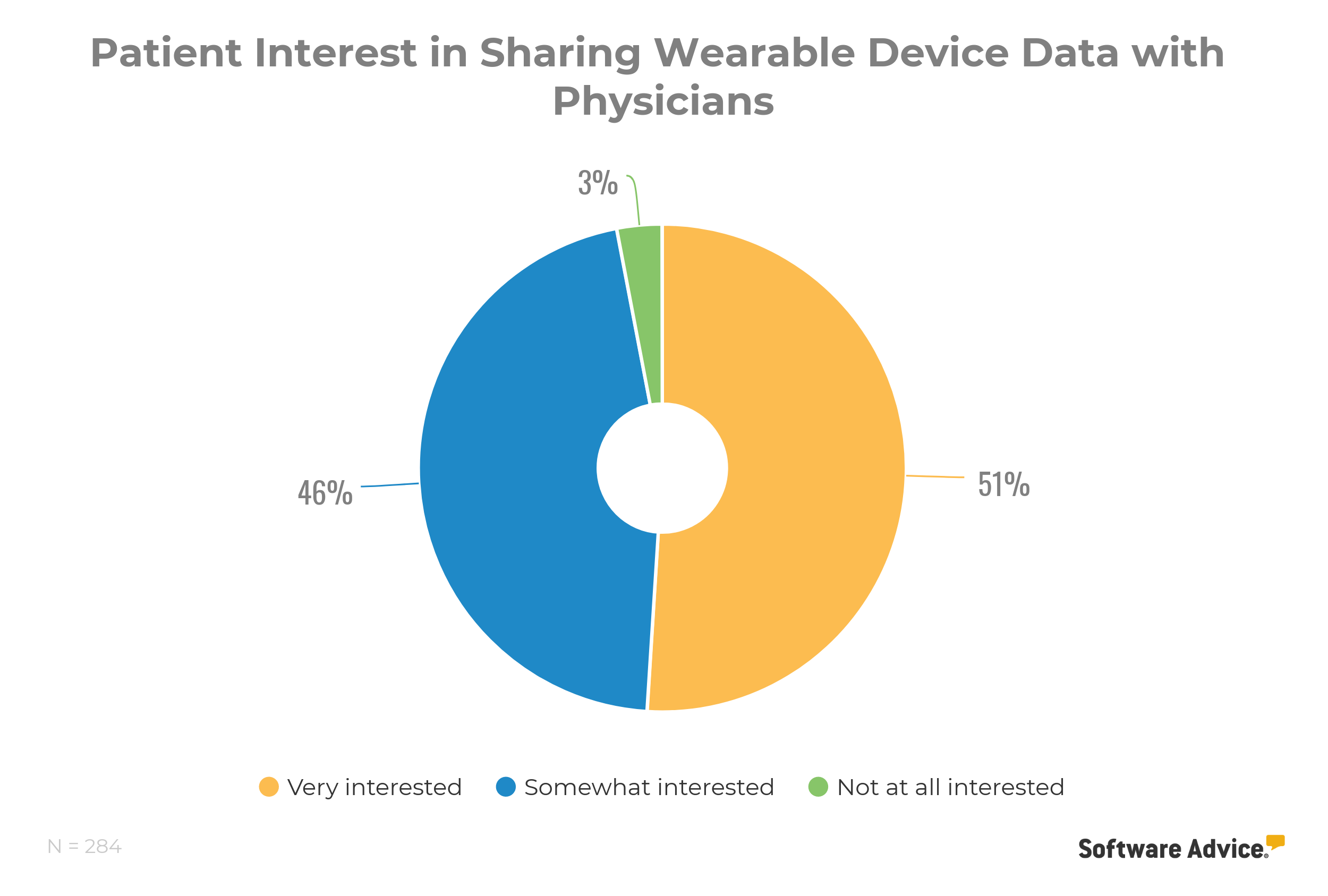
Our survey also revealed that 92% of patients who use fitness trackers will be more likely to select a doctor who asks about that data over a doctor who does not, indicating that patients want doctors to care about the data they collect with personal devices.
2. Waiting rooms will be phased out
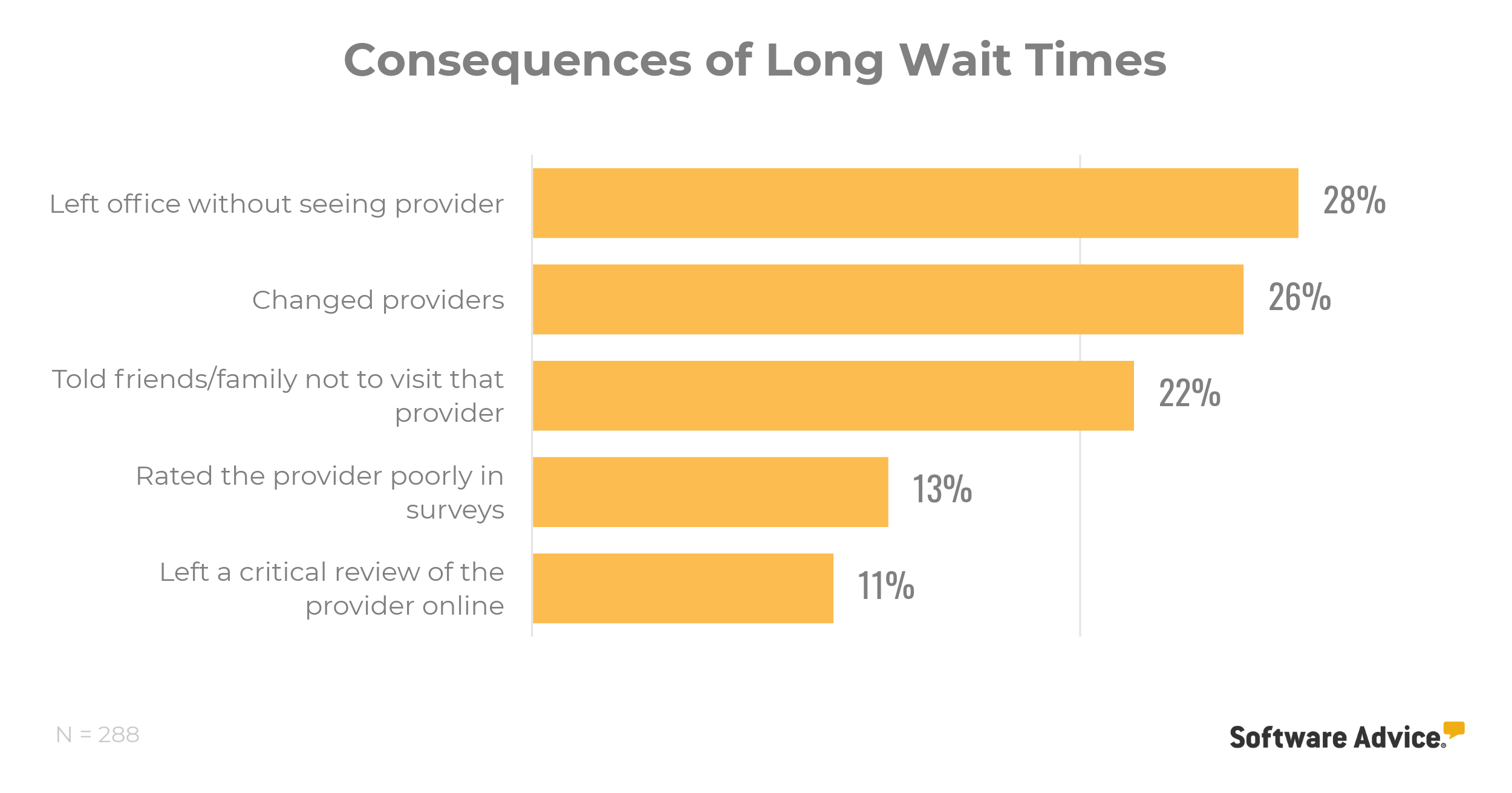
Talk to any patient and they’ll agree that they prefer less time spent in the waiting room. In fact, another Software Advice survey of over 300 patients in the U.S. found that doctors who do not take steps to reduce wait times stand to lose over half of their patient base in a year.
Although the waiting room experience has already become more streamlined with advances such as online check-ins, experts say waiting rooms will continue to become more efficient in the future, or will even disappear altogether.
Geeta Nayyar, chief medical officer at Greenway Health, believes the waiting room will continue to exist, but that the time patients spend at the doctor’s office will be used more efficiently. “The visit will start right when you walk in the door,” she says.
“For example, the provider might see that you have diabetes that requires a certain type of screening. If you complete the screening in the waiting room and test positive, that information can be sent directly to the doctor to make the visit more efficient.”
And that’s good news—especially when you consider the potential consequences of long wait times.
Patients filling out pre-visit forms online coupled with data transmitted from wearable technology could give doctors most, if not all, the information they need in advance.
Less time spent collecting background information means the visit can be devoted solely to the patient’s current ailment or issue. This can greatly speed up the duration of appointments and reduce—or even eliminate—the need for wait times and waiting rooms.
3. Up to a quarter of visits will happen virtually
Traveling to the doctor’s office for a routine checkup can consume a decent chunk of your day. While these visits are important for ensuring your ongoing health, the future offers a more efficient and less time-consuming solution: telemedicine.
More and more patients are taking advantage of telemedicine to connect with doctors via video chat, and some are currently able to order new prescriptions through patient portals, saving them a trip to the doctor’s office. Over the next decade, this trend is expected to rise.
Dr. Natasha Burgert, a pediatrician who frequently blogs about the patient-doctor connection, also sees the value in remote medical treatment as it allows doctors to easily interact with and treat patients with minor ailments. “If I looked at my schedule today, somewhere between 10% to 20% of the visits could be conducted through telemedicine,” she estimates.
We’re also excited about the potential of telemedicine to change the way healthcare is provided. Over the years, we’ve conducted several surveys, each monitoring patient sentiment around telemedicine and virtual care, and we’ve seen a markable trend towards more patient awareness and use of telemedicine. We also found that 81% of patients would choose a doctor who offers telemedicine over one who doesn’t.
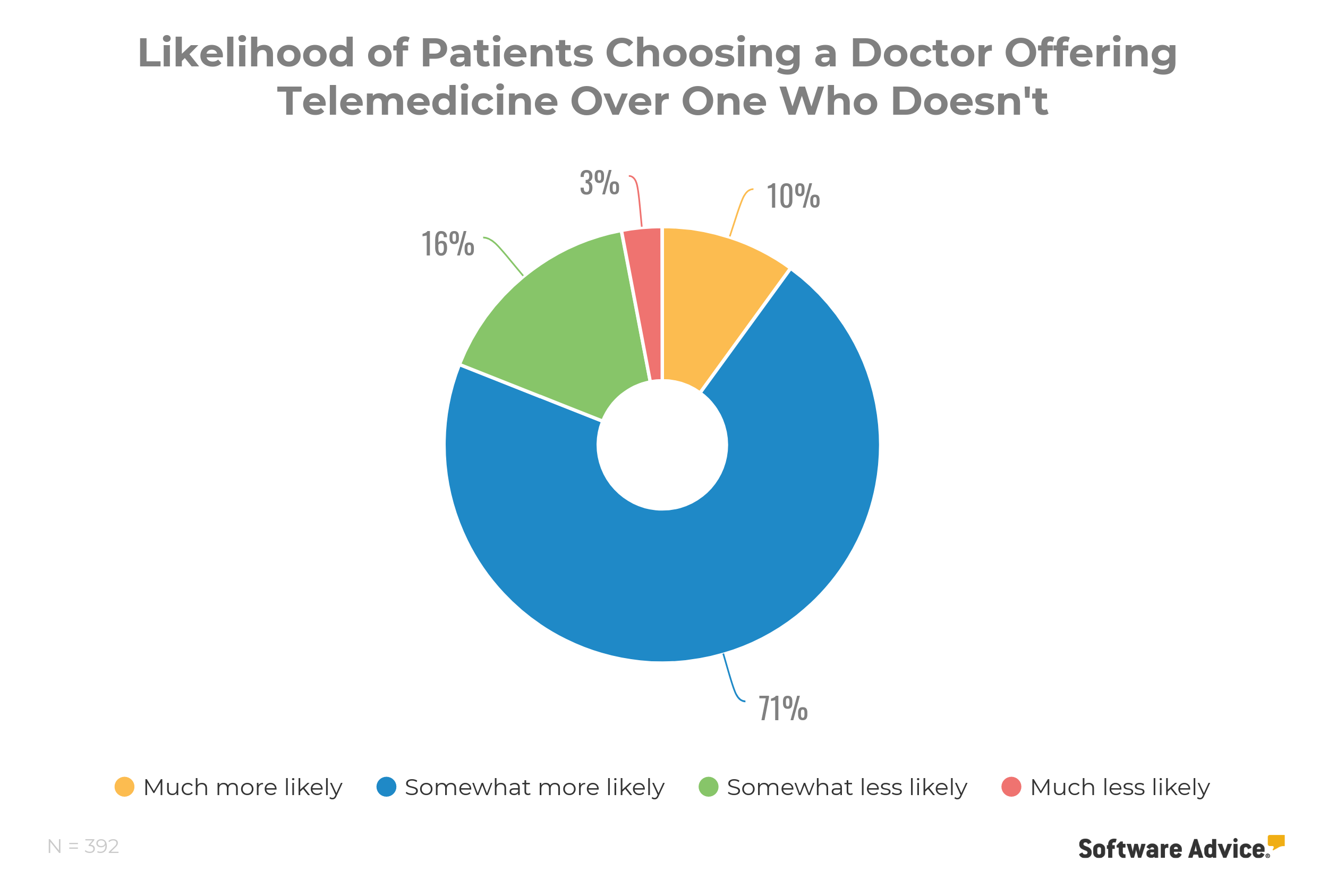
Considering the fact that 96% of U.S. hospitals have plans to provide more telemedical services to patients in the coming year, we fully expect to see virtual appointments become as commonplace as actual trips to the doctor’s office have been in the past.
4. Patients will take more ownership of their personal health data
According to a survey from Wolters Kluwer Health, 80% of patients want greater control over their own healthcare, but only 19% have access to a personal health record. In the future, patients and doctors could satisfy this demand by charting their visits together. In fact, some modern radiology information systems and picture archiving and communications systems (PACS) already exemplify a step in the direction of patient control.
Charting the visit together would allow patients to share more of their story. Patients often share a lot of detail during their visit with their doctor, much of which is lost during the note-taking process.
“Patients really want their story to be heard, but as they tell that story, it’s very difficult for us to translate that story into our electronic records,” Burgert explains.
But in the future, Burgert imagines that new technology could include a simple series of questions with drop-down menus and comment boxes that could be uploaded into the patient’s EMR.
This survey or intake form could be emailed to the patient a few days prior to their appointment and the results pre-loaded into the system. The doctor could then read the form prior to the visit, ask relevant questions when they are with the patient, and then add to the narrative as they see fit.
“It would allow the time with the doctor to be more efficient, with less frank ‘data collection’ and more supportive questioning,” Burgert says. “This would optimize face time with the patient and optimize the use of a skilled practitioner’s time, allowing better assessment and plan discovery for both doctor and patient. It would also allow more time for the patient to engage in self-assessment by committing their story to paper, possibly even facilitating more honesty in the medical record.”
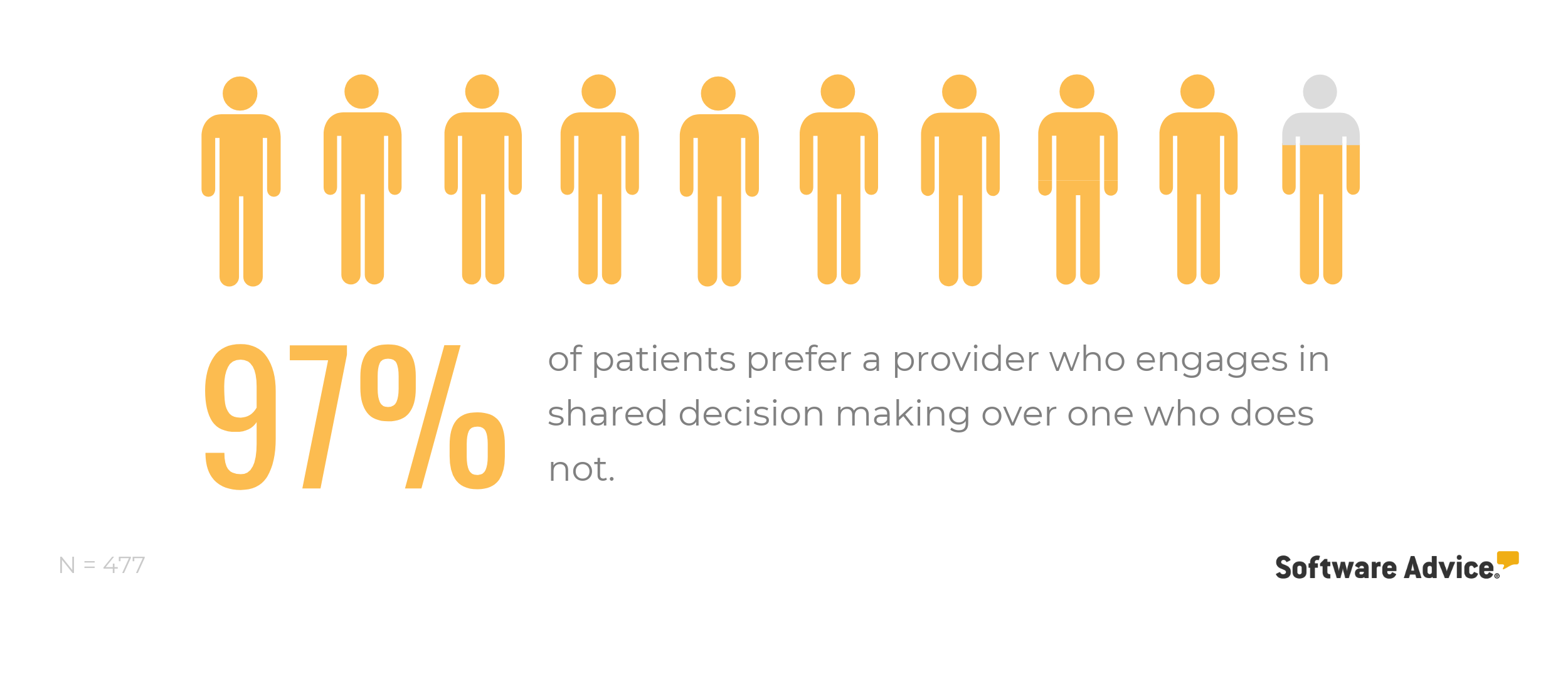
Similarly, we ran a survey to learn how patients felt about shared decision making as an avenue to achieve more control of their healthcare, and we found (unsurprisingly) that patients appreciate the idea.
How to prepare for medical technology of the future
It’s clear there are many exciting developments on the horizon that will change the way doctors and patients interact in primary care practices. While all changes require some type of adjustment, there are a few steps that doctors can take now to get a head start.
➔ Get involved in professional associations. Nayyar explains that professional associations often have the latest and greatest information relevant to your particular specialty. She also recommends speaking to colleagues to find out what worked and didn’t work for them so you can use this information to invest wisely in different types of technology for your own practice.
➔ Listen to your patients. Healthcare is continuing to evolve into a consumer-driven space. If your patients express a desire to be more involved in their care, spend less time in the waiting room, or have the ability to email or text you with questions related to their care, you should start thinking about how to integrate technologies into your practice that will enable this.
➔ Embrace new technology. As new technology becomes more widespread in healthcare, patients are likely to not only embrace it, but seek out physicians who are using it. Learning and adopting this technology early on will put you ahead of the curve. Burgert explains that much of this emerging technology is how doctors will maintain their relevance and gain new patients in the future—and ultimately, avoid becoming “obsolete.”
The key for success, Burgert says, is for physicians to push through the learning curve and any anxiety associated with new technologies and be open to the changes that lie ahead. She explains: “Physicians who maintain their willingness to listen and learn, despite the common anxiety of not knowing everything in uncharted territory, will be better positioned in the future.”
To learn more about medical technology for your practice, check out these resources: